VA North Texas health care
At VA North Texas Health Care System, our health care teams are deeply experienced and guided by the needs of Veterans, their families, and caregivers. Find a health facility near you, and manage your health online. Sign up for community events and updates.
Locations
Garland VA Medical Center

Sam Rayburn Memorial Veterans Center
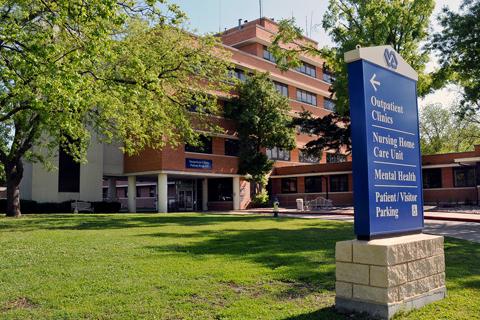
Dallas VA Medical Center

Manage your health online
In the spotlight at VA North Texas health care
Stories
One Veteran’s story of going from substance abuse to sobriety
A Veteran’s journey of hope and redemption.


